SEE ALSO:
Infectious Diseases and Outbreaks
STD Division
NEED HELP?
Having trouble finding what you are looking for? Use our A to Z Index.
For Healthcare Providers
The Mpox Consultation Form is no longer required for submission of specimens to the state public health laboratory (SPHL) for testing.
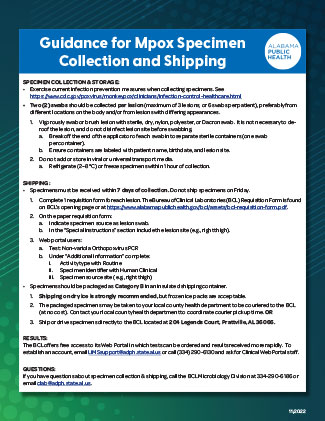
At this time, testing for mpox can be performed by various laboratories across the state, including public health, commercial, and some clinical/research laboratories. The Alabama Department of Public Health is available to assist with mpox testing. If your patient is suspected of having mpox and you wish to use our public health laboratory's services, please download the Guidance for Mpox Specimen Collection and Shipping.
If you are a vaccination provider, please visit our For Vaccination Providers page.
Table of Contents
- What's New?
- HAN Alerts
- Additional Resources
- Children and Adolescents
- Pregnancy and Breastfeeding
- Therapeutics
- Vaccine
What's New?
- Mpox Updates for Clinicians (CDC) (December 2023)
- MMWR- Mpox in Adults Aged >50 Years -United States, May 2022- May 2023
- MMWR - Exposures to Mpox Among Cases in Children - United States, September-December 2022
- MMWR - Effectiveness of JYNNEOS Vaccine Against Diagnosed Mpox Infections - 2022
- Interim Clinical Treatment Considerations for Severe Manifestations of Mpox — United States, February 2023
- MMWR - Ocular Mpox — United States, July–September 2022
- CDC/IDSA Call - Mpox: Updates on Testing, Vaccination, and Treatment (July 23, 2022)
- Mpox Virus Planning Response (Video)
- Dr. Walensky's Dear Colleagues Letter for Clinicians
- WHO Meeting of the International Health Regulations Emergency Committee
- Interim Clinical Considerations for Use of JYNNEOS and ACAM2000 Vaccines during the 2022 U.S. Mpox Outbreak
HAN Alerts
- 11/19/24- First Case of Clade 1 Mpox Diagnosed in the United States
- 11/21/22 - CDC Updates Guidance for Clinicians Treating Patients at Risk for Severe Mpox Disease
- 10/04/22 - Mpox Update
- 09/28/22 - Testing for Mpox (MPX) in Jefferson County
- 08/31/22 - Mpox Update
- 08/02/22 - Mpox Situation Update
- 07/18/22 - Testing for Mpox (MPX) in Jefferson County
- 07/08/22 - Guidance for Mpox Test Submission
- 06/18/22 - CDC and ADPH Health Advisory on Mpox Virus Infections in the United States and Other Non-endemic Countries – 2022
- 05/26/22 - UPDATED with additional Epidemiologic, Clinical, and Exclusion Criteria: CDC and ADPH Health Advisory on Mpox Virus Infections in the United States and Other Non-endemic Countries - 2022
- 05/23/22 - CDC and ADPH Health Advisory on Mpox Virus Infections in the United States and Other Non-endemic Countries - 2022
Visit the Health Alert Network (HAN) for CDC's HAN Messages.
Additional Resources
- Infection Prevention and Control of Mpox in Healthcare Settings (CDC)
- CDC Isolation and Control at Home
- Diagnostic Process for Mpox Virus Testing (CDC)
- What Clinicians Need to Know About Mpox in the United States and Other Countries (CDC | Updated June 2022)
- Mpox: What Clinicians Need to Know (HIVMA)
- Mpox in the U.S.: An Update for Clinicians and the LGBTQ+ Community (Recording) (IDSA)
- National Emerging Special Pathogens Training and Education Center (NETEC): Mpox
ACIP Meeting Presentations
More presentations are available at the ACIP Meetings.
Children and Adolescents
Mpox should be considered when children or adolescents present with a rash that could be consistent with the disease, especially if epidemiologic criteria are present. Young children, children with eczema and other skin conditions, and children with immunocompromising conditions may be at increased risk of severe disease. Treatment should be considered on a case-by-case basis for children and adolescents with suspected or confirmed mpox who are at risk of severe disease or who develop complications of mpox. Tecovirimat is the first-line medication to treat mpox, including in children and adolescents. Children and adolescents exposed to individuals with suspected or confirmed mpox may be eligible for post-exposure prophylaxis (PEP) through vaccination, immune globulin, or antiviral medication. For more information, read:
- Clinical Considerations for Mpox in Children and Adolescents
- Update for Clinicians on Mpox in People with HIV, Children and Adolescents, and People who are Pregnant or Breastfeeding
Pregnancy and Breastfeeding
Data regarding mpox infection in pregnancy are limited. It is unknown if pregnant people are more susceptible to the mpox virus or if the infection is more severe during pregnancy. The mpox virus can be transmitted to the fetus during pregnancy or to the newborn by close contact during and after birth. Adverse pregnancy outcomes, including spontaneous pregnancy loss and stillbirth, have been reported in cases of confirmed mpox infection during pregnancy. Preterm delivery and neonatal mpox infection have also been reported. The frequency and risk factors for severity and adverse pregnancy outcomes are not known. For more information, read:
- Clinical Considerations for Mpox in People Who are Pregnant or Breastfeeding
- Update for Clinicians on Mpox in People with HIV, Children and Adolescents, and People who are Pregnant or Breastfeeding
Therapeutics
There are no treatments specifically for mpox virus infections. However, mpox and smallpox viruses are genetically similar, which means that antiviral drugs and vaccines developed to protect against smallpox may be used to prevent and treat mpox virus infections.
Antivirals, such as tecovirimat (TPOXX), may be recommended for people who are more likely to get severely ill, like patients with weakened immune systems. For information concerning mpox therapeutics and obtaining TPOXX, read:
- Treatment Information for Healthcare Professionals
- Information for Healthcare Providers on Obtaining and Using TPOXX (Tecovirimat) for Treatment of Mpox
Vaccines
Two vaccines may be used for the prevention of mpox virus infection:
- JYNNEOS (also known as Imvamune or Imvanex), licensed (or approved) by the U.S. Food and Drug Administration (FDA) for the prevention of mpox virus infection, and ACAM2000, licensed (or approved) by the FDA for use against smallpox and made available for use against mpox under an Expanded Access Investigational New Drug application.
- No data are available yet on the effectiveness of these vaccines in the current outbreak.
- The immune response takes 14 days after the second dose of JYNNEOS and 4 weeks to reach its maximum development.
- People who get vaccinated should continue to take steps to protect themselves from infection by avoiding close, skin-to-skin contact, including intimate contact, with someone who has mpox.
- To better understand the protective benefits of these vaccines in the current outbreak, the CDC will collect data on adverse events and vaccine effectiveness, including whether the vaccine provides protection differently depending on how a person was infected with the mpox virus.
For more information, read Considerations for Mpox Vaccination.
Page last updated: February 12, 2026
SEE ALSO:
Infectious Diseases and Outbreaks
STD Division
NEED HELP?
Having trouble finding what you are looking for? Use our A to Z Index.